What You Should Know About Joint Replacement Surgery

Chances are you know someone who has undergone joint replacement surgery. These surgeries, most often involving knees and hips, have become increasingly common, with more than one million performed in the United States each year.

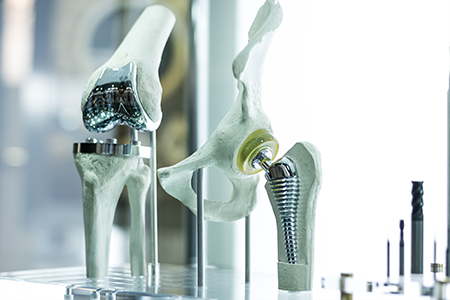
Usually, a joint is replaced because it has been damaged by arthritis or an injury and is the cause of significant pain. Some or all of the damaged joint is removed during surgery and replaced with a prosthesis. A prosthesis is a metal, ceramic, or plastic device designed to replicate the movement of a healthy, normally functioning joint.
While knee and hip replacements are most common, surgery can be performed on other joints, including the elbow, ankle, wrist, and shoulder.
We sometimes think of joint replacement as a recent medical innovation, but the technique has been used in some form for 130 years. The first hip replacement was attempted in Germany in 1891 by a doctor who used ivory devices to replace femoral heads in patients whose hip joints were destroyed by tuberculosis.
While these early attempts were not particularly successful, surgeons continued to advance their techniques. Sir John Charnley, a British orthopedic surgeon who designed a prosthesis in the early 1960s that is nearly identical to those used today, is considered the father of the modern hip replacement.
About a decade later, the condylar knee prosthesis was developed, and total knee replacements became increasingly common. Today, they are one of the most common elective surgeries.

Knowing if You Need a Joint Replacement
Joint replacement surgery is not for everyone, as there are less drastic treatments such as physical therapy, weight loss, and medication to try first. If you’ve tried and found nonsurgical treatments are not working, and your damaged joint makes it difficult for you to accomplish daily tasks, sleep, or participate in activities you enjoy, then you may want to talk to your doctor about joint replacement.
Your primary care provider will assess your symptoms and recommend a consultation with an orthopedic surgeon or rheumatologist to determine whether you are a candidate for surgery. X-rays, CT scans, or an MRI may be used to document the severity of joint damage and plan a course of treatment.
Patients usually considered eligible for joint replacement surgery are in good health other than the joint problem and experience high levels of chronic pain caused by osteoarthritis. The Rothman Orthopedic Institute, a leading orthopedic practice based in Philadelphia, recommends a five-question self-test to determine whether joint replacement may be a good option:
- Can I live with the pain I am currently experiencing?
- Have my symptoms (mainly pain) worsened over the past year?
- Am I healthy enough for surgery?
- Am I prepared to undertake the recovery process?
- Will my insurance cover the procedure and costs associated with rehab?
If you are considering joint replacement, consider how you answered those questions. Discuss your situation with your doctor and family members.
Preparing for Joint Replacement Surgery
There are steps you can take to prepare for joint replacement surgery in order to have a successful outcome, and ConnectCare3’s Nurse Navigators are here to support you along the way. Your Nurse Navigator will help to identify well-qualified surgeons with a specific background in joint replacements and provide you with additional tools and resources so you are able to make well-informed decisions about your procedure. Keep in mind that surgeons who perform high-volumes of a specific procedure tend to have better outcomes, so it will be important to select a physician with this level of expertise.
You should receive detailed instructions from the medical group that will perform your surgery. Be sure to read the instructions carefully and contact your doctor right away if there is something that you do not understand.
In some cases, physical therapy is recommended before surgery to help strengthen muscles around the joint. If you take certain medications, you may be advised to stop them several days before surgery.
You will be advised not to eat or drink anything for a certain number of hours before surgery. You may be instructed to disinfect your skin with special cloths or soap provided by your surgeon.

What to Expect Before and After Surgery
Before your surgery, you can expect:
- A medical team to prepare you for surgery and discuss anesthesia
- Receive anesthesia, a sedative, and an intravenous antibiotic to reduce the chance of infection
After your surgery, you can expect:
- Assistance with standing or walking
- Minimal physical therapy in the hospital to aid you in completing day to day tasks
- Instructions for exercises at home and physical therapy recommendations
- Information on medication

Readying Your Home for Recovery
You can make your home as safe as possible during your recovery period by taking steps before your surgery. The Mayo Clinic recommends the following actions to create a secure environment as you recover for lower extremity replacements:
- Create a living space on one floor since climbing stairs can be difficult
- Install safety bars or a secure handrail in your shower or bath.
- Secure stairway handrails
- Get a stable chair with a firm seat cushion and back and a footstool to elevate your leg
- Arrange for a toilet-seat riser with arms if you have a low toilet
- Get a stable bench or chair for your shower
- Remove loose rugs and cords

Recovering After Surgery
You will be advised to continue exercising on your own or participating in physical therapy after returning home. You should be able to resume most daily activities within three to six weeks, assuming no complications. Your doctor will advise you about driving, but you should not drive if you are taking narcotic pain medications.
Most people respond well to joint replacement and experience pain relief, improved mobility, and better quality of life. The age at which patients receive joint replacements has lowered in recent years. Better technology assures prostheses last longer and perform better. If you are severely hindered by joint pain, joint replacement surgery may be a valid consideration

Caring for Your Joints
Of course, caring for your joints in the first place can help reduce the possibility that you’ll require joint replacement surgery. To do so, experts recommend getting plenty of exercise and eating a diet rich in calcium, Vitamins D and C, and protein.
You should protect your joints during activity, build muscles to support your joints, exercise for a strong core, and keep your weight at a healthy level. Avoid activities that over-stress your joints, and practice good posture, which helps to protect your joints.

Utilizing ConnectCare3
If your physician advises you that you should undergo joint replacement surgery, reach out to ConnectCare3. Our Nurse Navigators can research and prepare a list of well-qualified physician options for you to consider, especially if you are thinking about getting a second opinion. Our Nurse Navigators can also help to prepare you for upcoming appointments and your procedure by providing a list of questions for you to review with your surgeon.

Download the Free Resource
Access a printer-friendly version of the resource to reference later.